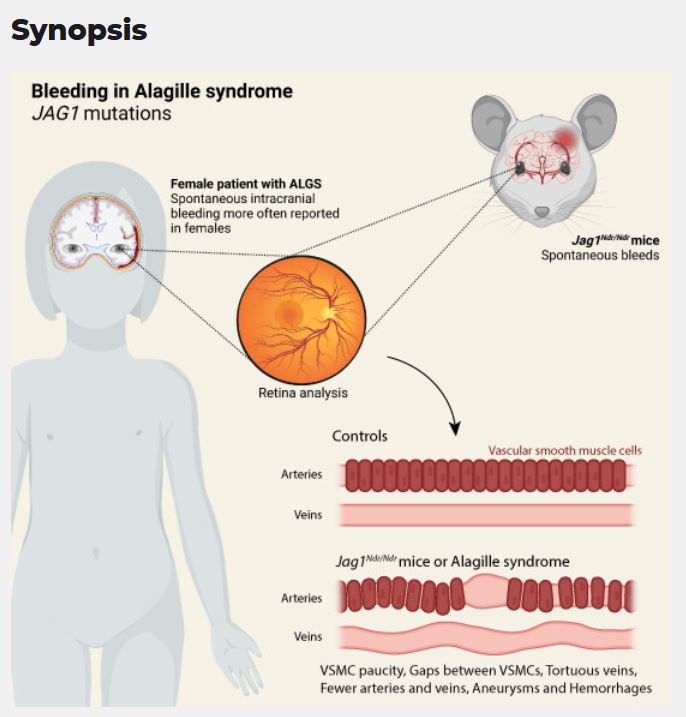
Abstract: Spontaneous bleeds are a leading cause of death in the pediatric JAG1-related liver disease Alagille syndrome (ALGS). We asked whether there are sex differences in bleeding events in patients, whether Jag1Ndr/Ndr mice display bleeds or vascular defects, and whether discovered vascular pathology can be confirmed in patients non-invasively. We performed a systematic review of patients with ALGS and vascular events following PRISMA guidelines, in the context of patient sex, and found significantly more girls than boys reported with spontaneous intracranial hemorrhage. We investigated vascular development, homeostasis, and bleeding in Jag1Ndr/Ndr mice, using retina as a model. Jag1Ndr/Ndr mice displayed sporadic brain bleeds, a thin skull, tortuous blood vessels, sparse arterial smooth muscle cell coverage in multiple organs, which could be aggravated by hypertension, and sex-specific venous defects. Importantly, we demonstrated that retinographs from patients display similar characteristics with significantly increased vascular tortuosity. In conclusion, there are clinically important sex differences in vascular disease in ALGS, and retinography allows non-invasive vascular analysis in patients. Finally, Jag1Ndr/Ndr mice represent a new model for vascular compromise in ALGS.
Spontaneous bleeds are a significant cause of death in the rare genetic disease Alagille syndrome, but little is known about the risk factors contributing to the bleeding events, or about vascular development and maintenance in the course of the disease.
- Alagille syndrome is modeled by Jag1Ndr/Ndr mice, including high mortality and sporadic bleeding.
- More female than male patients with Alagille syndrome are reported with intracranial bleeds, and certain vascular phenotypes are more severe in female Jag1Ndr/Ndr mice.
- Bleeding risk in Jag1Ndr/Ndr mice may be further modified by thin skull bones, fragile vascular smooth muscle cells, premature vascular aging, and increased venous tortuosity.
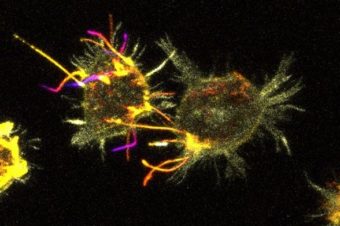
- Developmental and homeostatic vascular defects were detected in both endothelial cells and vascular smooth muscle cells in Jag1Ndr/Ndr mice.
- The vascular defects observed in Jag1Ndr/Ndr mice could be visualized, quantified, and validated in retinographs from patients, suggesting a non-invasive method to assess vascular health.
Authors:
Simona Hankeova 1,2, Noemi Van Hul 1, Jakub Laznovsky 3, Elisabeth Verboven 1, Katrin Mangold 1, Naomi Hensens 1,4, Csaba Adori 5, Elvira Verhoef 1,4, Tomas Zikmund 3, Feven Dawit 6, Michaela Kavkova 3, Jakub Salplachta 3, Marika Sjöqvist 1, Bengt R Johansson 7, Mohamed G Hassan 8,9, Linda Fredriksson 10, Karsten Baumgärtel 11, Vitezslav Bryja 2, Urban Lendahl 1, Andrew Jheon 8, Florian Alten 12, Kristina Teär Fahnehjelm 13,14, Björn Fischler 6, Jozef Kaiser 3, Emma R Andersson 1
- 1 Department of Cell and Molecular Biology, Karolinska Institutet, Stockholm, Sweden.
- 2 Department of Experimental Biology, Masaryk University, Brno, Czech Republic.
- 3 CEITEC – Central European Institute of Technology, Brno University of Technology, Brno, Czech Republic.
- 4 University of Applied Sciences Utrecht, Utrecht, The Netherlands.
- 5 Department of Neuroscience, Karolinska Institutet, Stockholm, Sweden.
- 6 Department of Pediatrics, Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet and Karolinska University Hospital, Huddinge, Sweden.
- 7 EM Unit, Institute of Biomedicine, University of Gothenburg, Gothenburg, Sweden.
- 8 University of San Francisco, San Francisco, CA, USA.
- 9 Department of Orthodontics, Faculty of Dentistry, Assiut University, Assiut, Egypt.
- 10 Department of Medical Biochemistry and Biophysics, Karolinska Institutet, Stockholm, Sweden.
- 11 Travere Therapeutics, San Diego, CA, USA.
- 12 Department of Ophthalmology, University of Muenster Medical Center, Münster, Germany.
- 13 Department of Pediatric Ophthalmology, Strabismus, Electrophysiology and Ocular Oncology, St. Erik Eye Hospital, Karolinska Institutet, Stockholm, Sweden.
- 14 Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden